Captive Insurance Overview: Healthcare Provider Industry Highlights
Mar 15, 2019
Healthcare provider captive insurance arrangements represent approximately 15% of the global captive insurance market and are currently one of the largest growing sectors within the captive industry due to the changing risk landscape that healthcare organizations are facing. Approximately 75% of hospitals now have some form of alternative risk management in place for their professional liability insurance and over 60% of funding for liability exposures for healthcare providers is now through non-traditional coverages. The growth of alternative risk management within the healthcare industry is driven by several varying factors including the cost efficiencies gained through the use of the wholesale reinsurance market over the cost of the commercial market place; the consolidation of provider organizations and the change from a fee-for-service payor model to a value-based care model; and the emerging risks facing provider organizations as the healthcare landscape changes.
Access to Reinsurance Markets
Captive insurance companies are actual insurance companies that are regulated by state departments of insurance and, as such, they can access the wholesale reinsurance market that is typically not available to healthcare provider organizations. Healthcare professional liability or medical malpractice coverage is one of the most common coverages seen in healthcare captives, and the traditional medical malpractice market has historically been prohibitively expensive with limited capacity to cover the needs of healthcare organizations.
Access to the reinsurance markets allows these captives to negotiate with wholesale reinsurers either directly or through brokers for more favorable terms and premium rates compared to the commercial market due to the additional capacity and competition present within the reinsurance market.
Better Management of Patient Care
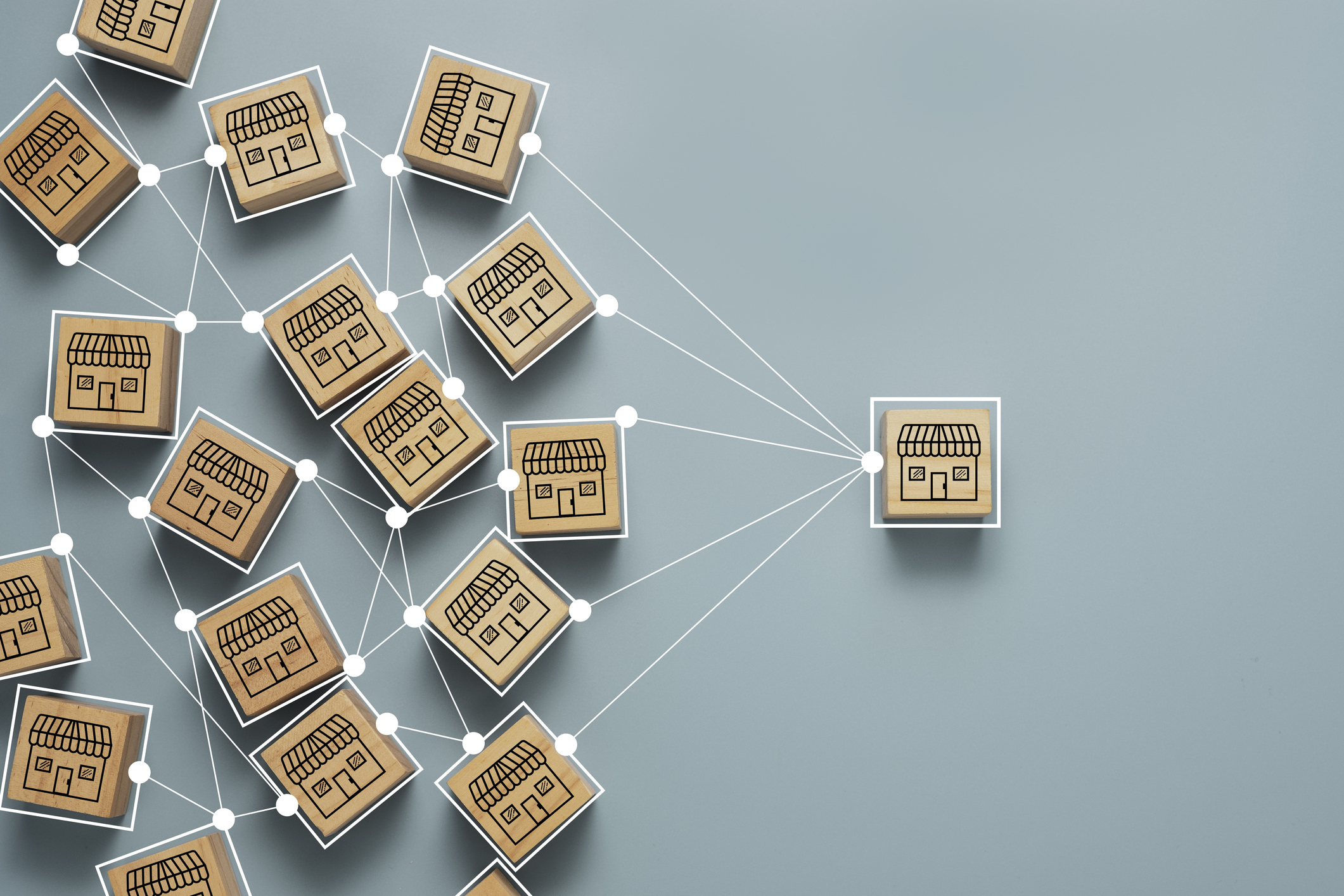
The rapid consolidation within the healthcare industry and the change in the payor model within the healthcare system in the United States make the use of captives more prevalent and more beneficial to healthcare provider organizations. The consolidation has come in the form of health system mergers, but also from rapid consolidation of private physician practices and physician groups into hospital organizations in order to join accountable care organizations (ACOs), health maintenance organizations (HMOs), and other managed care groups as the payor model for providers moves towards a population management approach requiring health systems to align with their physicians closely. In fact, since 2016, more physicians have been employed by hospitals than were in private practice, with that ratio currently around 60%. This allows provider captive programs to increase their risk pooling due to the additional risks from those physician groups as they leave the commercial market place and enter provider captive programs.
Additionally, with the implementation of the healthcare reform laws, much more emphasis is placed on the quality of care and the payor model changing from a largely fee-for-service based payor model to an outcome-based compensation model with more focus on overall population health management through the use of capitation contracts for healthcare providers organizations. Under capitation contracts, organizations are paid a set dollar amount per patient per month without regards to how much care and service that patient requires. This payment structure is designed to require providers to prioritize outcomes of service over the quantity of procedures provided creating enhancements in patient safety and experiences and increasing the efficiency of our healthcare system. As this fee structure changes, more emphasis needs to be placed on the quality of patient care.
Many healthcare organizations have found that they have very competent and sound risk management and quality management departments, but that those two departments generally have limited communication and information sharing between themselves. Healthcare captives underwriting professional liability, an excess of loss, or other coverages contain a wealth of historical claims data related to patient failures, lapses in care, and other safety failures which can be used to bridge the gap between risk and quality management. These coverages provide quality management departments with the information they need to better manage their quality of care in order to limit readmissions and excess patient care to increase overall operating margin. In fact, this benefit in healthcare captives is greater than ever due to the increased size of many captive programs caused by the consolidation within the industry. This has led to the increased pooling of risks and volume of claims information available to be analyzed within the captive programs for use in quality improvement measures.
The emergence of capitation contracts causes provider organizations to assume the risk of patient health and risk a monetary loss if the cost of care exceeds the funds provided in the contract. A captive insurance company can be utilized to fund these future expected losses on capitation contracts as a means for stabilizing healthcare providers’ profits and cash flows using provider excess of loss coverages placed on the capitation contracts entered into by the healthcare organization. Contact your CRI professional to learn more about how you can utilize a captive insurance company to better manage your organization.