The Evolution of Healthcare Finance, Post-Pandemic
- Contributor
- Bryan Hall
Jul 28, 2023
The healthcare industry has been on a roller-coaster ride since the beginning of the COVID-19 pandemic. An event of unprecedented scale, the pandemic not only tested the resilience of our healthcare infrastructure but also induced rapid changes in the landscape of healthcare finance.
The pandemic's financial implications were, and continue to be, staggering. According to a study by Harvard University, the estimated total cost of the pandemic stands at a jaw-dropping $16 trillion - before accounting for the stimulus bills enacted under President Biden. To put this into perspective, the estimated cost of the pandemic is more than three times the cost of World War II, which totaled approximately $5 trillion, adjusted for inflation.
Dire Consequences for Healthcare Providers
The pandemic had devastating impacts on healthcare providers, with alarming reductions in service volume, particularly outpatient services, which have yet to recover fully. The mortality rate among healthcare workers, most notably in post-acute care settings, was heart wrenching.
From a financial perspective, unprecedented wage growth in nursing has further strained the already-fragile healthcare system, exacerbated by staffing and capacity constraints, margin erosion, cash flow issues, supply chain disruptions and unmanageable inflation.
While the financial burden of the pandemic has been wide-reaching, it has not been evenly distributed. Large health systems, primarily academic and charity facilities, skilled nursing facilities, and providers reliant on outpatient visits, bore the brunt of the crisis.
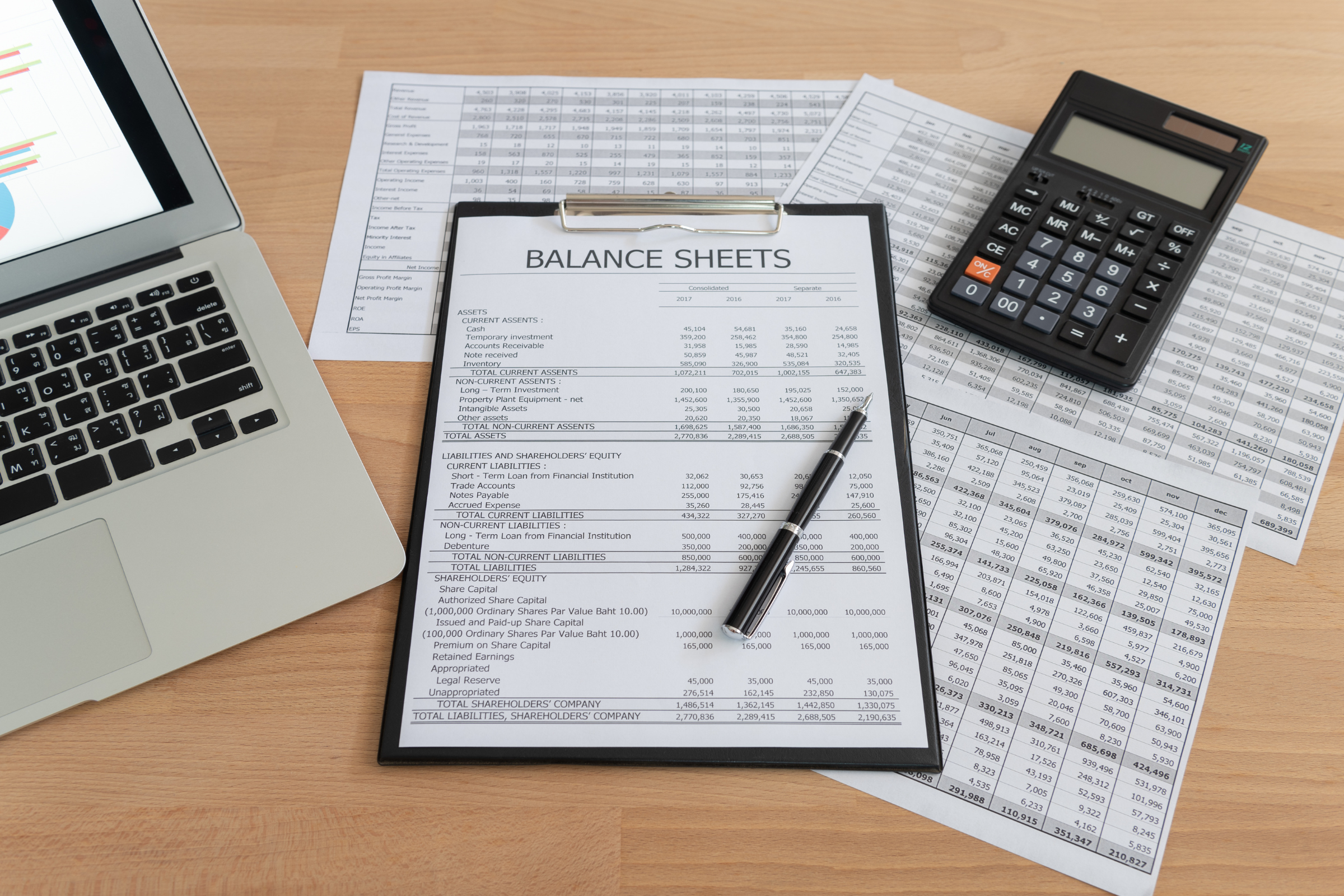
Financial Challenges and Cash Flows in Healthcare
As we move forward in the post-pandemic era, several challenges continue to persist, shaping the new financial landscape of the healthcare industry. While COVID-19 admissions decrease to near zero, wage costs continue to soar (or remain at elevated levels). Both inpatient and outpatient volumes typically remain at or below pre-pandemic levels, indicating a sustained drop in healthcare service usage.
Furthermore, the Coronavirus Aid, Relief, and Economic Security (CARES) Provider Relief Fund (PRF) is exhausted. Adding to this financial burden, repayment of the Medicare accelerated payments has significantly impacted the cash position of most healthcare facilities.
Wage inflation was a prominent feature of 2020 - 2022, with annual nursing wages increasing by 25-50% at many facilities. Because this wage escalation is unlikely to “normalize” in the near term, it will likely take several years of adjustments, suggesting a permanent wage increase and a "new normal" in the healthcare labor market.
Changing Dynamics for Patients and Providers
The COVID-19 pandemic profoundly impacted the healthcare industry, potentially reshaping the healthcare model that existed prior to the pandemic. A shift towards a more digitally-centric approach could be the new path, although there is a (less likely) possibility of reverting to the traditional model after a period of time. This transformation may bring about the following changes:
- Obstacles for Rural and Safety-net Facilities: Facilities in rural areas and those acting as safety nets are likely to encounter the steepest hurdles in recovering from the pandemic. Costs for these institutions may not revert to pre-pandemic levels in the foreseeable future, if at all. With the exhaustion of federal and state intervention and reimbursement increases that helped mitigate heightened costs, these facilities now look to the (perhaps unlikely) prospect of further legislative intervention. The emergence of a newly mobile and highly competitive workforce presents an additional challenge for smaller facilities, who were already experiencing shrinking margins before the pandemic.
- Patient Safety and Regulatory Expectations: In a world transformed by the pandemic, increased demand for stringent patient safety protocols, especially concerning infection control, from patients and federal/state regulators is a near certainty. The end of temporary federal intervention and the potential for an increased tax burden, in light of the increased wage structure, may add to the pressures faced by healthcare providers.
- States and Medicaid Expansion: The experience of the pandemic and the federal response it precipitated have sparked renewed discussions around Medicaid expansion. It is anticipated that several states, including those in the South, will reconsider Medicaid expansion in some format.
Current State of Healthcare in 2023
In an unexpected turn, the Public Health Emergency (PHE) was terminated earlier than some anticipated, setting off a domino effect. PHE termination led to the withdrawal of the 20% Medicare Diagnosis Related Group (DRG) increase for COVID, increased Federal Medical Assistance Percentage (FMAP) for Medicaid, continuous Medicaid enrollment, and many other waivers and flexibility measures. As a direct result, millions of former Medicaid beneficiaries are losing health insurance coverage in 2023.
The financial landscape has grown increasingly challenging, with the credit market significantly tightening and the U.S. Prime Rate peaking at over 8%. Moreover, the Russell 2000's performance remained stagnant during the first quarter of 2023. These conditions set the stage for the resurgence of hospital closures, a flurry of credit downgrades in health system debt, C-suite turnover, and a record number of hospital defaults. A surge in merger and acquisition activities is possible, if not likely, in response to this turbulent atmosphere, as organizations strive to pool resources and weather the storm.Navigating the complexities of the evolving healthcare landscape in the wake of the COVID-19 pandemic is a formidable task, and the ripple effects of these shifts in healthcare aren't limited to hospitals and care facilities alone. Whether you're an individual or an organization, understanding the implications of these changes is vital. Contact your CRI advisor to help you navigate these changes and understand the significance of their impact on you or your organization. Our healthcare team is ready to help you confidently face the uncertainties of the new healthcare landscape and position yourself for future success.