Preparing for Third-Party Payer Audits
- Contributor
- Bryan Hall
Jan 5, 2021
Thanks to the Coronavirus Aid, Relief, and Economic Security (CARES) Act, hundreds of billions of dollars have flowed into the U.S. healthcare system, providing a much-needed salve to begin healing wounds inflicted by COVID-19. Unfortunately, along with those funds comes the very real possibility of an audit.
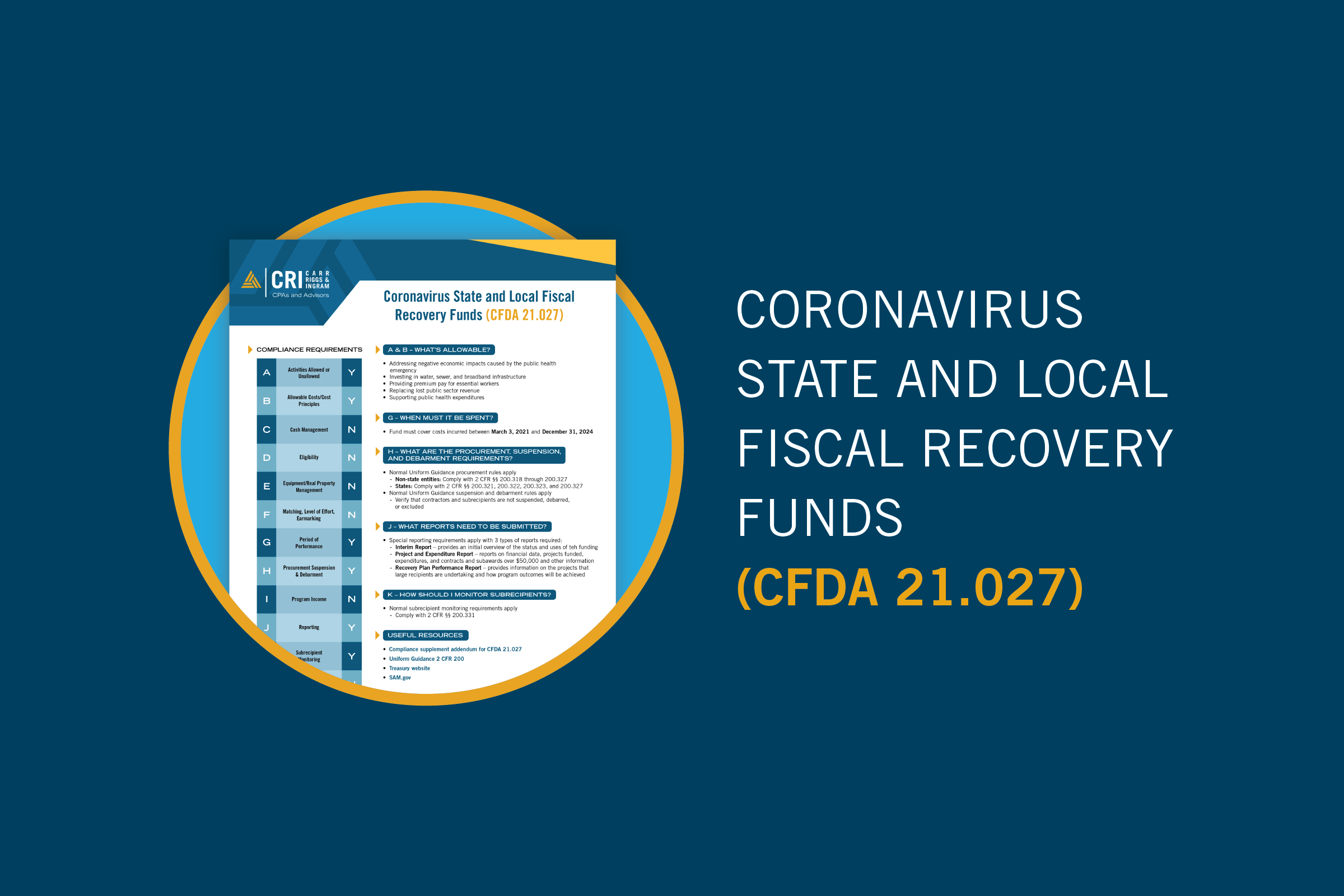
All providers that receive a total of $10,000 or more under the Provider Relief Fund (PRF) are required by the Department of Health and Human Services (HHS) to report their 2020 expenditures by February 15, 2020, with a follow-up report on 2021 expenses due July 31. Recipients “may be subject to auditing to ensure the accuracy of the data submitted to HHS for payment,” and those identified as having provided inaccurate information will be subject to payment recoupment and other legal action.
In addition, all PRF recipients awarded and expending more than $750,000 in a fiscal year are subject to the Uniform Administrative Requirements, Cost Principles, and Audit Requirements for federal awards — and that includes commercial (for-profit) entities as well as not-for-profit and governmental. This requirement means PRF recipients must submit to HHS either (1) a financial-related audit as defined in the Government Accountability Office “Yellow Book,” or (2) a so-called “Single Audit.”
Many PRF recipients have never been subject to a financial audit on the scale of a Yellow Book or Single Audit. However, most providers are all too familiar with the prospect of a payer audit.
Third-party payers have ramped up audit activity in recent years, even before the pandemic, and that scrutiny will only increase with the significant funding being distributed under the PRF and Paycheck Protection Program (PPP).
Document, Document, Document
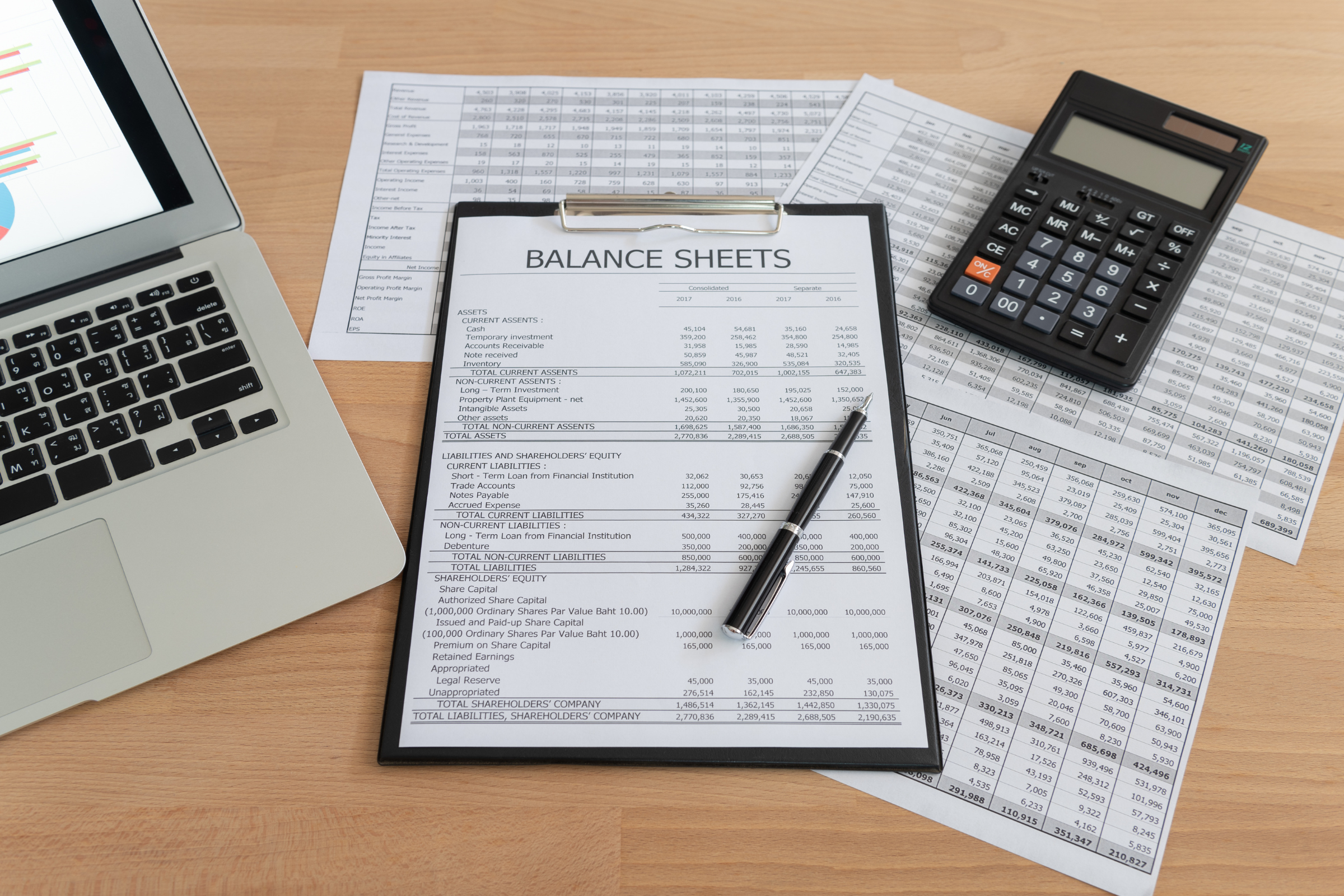
Any provider could be subject to an audit — whether by HHS, Medicare, a state Medicaid program, or even commercial payors — potentially leading to recoupment or denials that threaten the organization’s already thin, or negative, margins. The key to preparing and protecting your revenue streams from erosion or retroactive adjustments is to maintain thorough, accurate, easily accessible documentation.
In the case of federal awards like the PRF, you will need to maintain evidence — such as an invoice, timesheet, or journal entries — to support each and every cost or loss. HHS released a non-exhaustive list of allowable expenses, including such things as mortgage or rent for a medical office building, direct employee expenses for staff (including fringe benefits), lease payments on diagnostic equipment, PPE supplies, and IT expenses, such as for improved internet to support telehealth (all of the above subject to HHS’ specific guidelines).
PRF payments can be used toward any qualifying healthcare-related expense (subject to HHS’ specific guidelines) attributable to the coronavirus, as long as it is not reimbursed or obligated to be reimbursed from other sources. So, be prepared to show that you aren’t “double dipping” by using funds from multiple programs for the same expense —and this includes billings to patients or their insurance carriers.
Unlike all federal awards before it, PRF payments can make up for lost revenues. In its PRF FAQs, HHS says recipients can use any reasonable method of estimating lost revenue. For example, you could compare actual revenues to the same period last year. Or, if you had prepared a pre-pandemic budget, the estimated lost revenue could be the difference between budgeted revenue and actual revenue.
With most Medicare or commercial insurance audits, the primary focus is on billing and coding rather than revenue and expenses. In a retrospective audit, the payer may analyze a sample of medical files and expenses, and if they find even small discrepancies, they will dig deeper. These audits can lead to what the payer deems a pattern of inappropriate billing/reporting and ultimately what can amount to significant demands for repayment.
To successfully reverse a payer’s adverse decision, or reduce the repayment liability, providers must submit an appeal within the allowed timeframe and subsequently provide documentation that shows the billing was in compliance with the payer’s policies.
Review and Reconcile
Of course, the time to find any discrepancies — whether in billing practices or in costs and losses charged to a federal award — is before the bill, cost report, or other reporting is submitted. Review and reconcile expenditures as often as is practical and flag any transactions that appear “iffy” for further review.
Make sure that billing personnel and those who are responsible for charging costs to federal awards stay up to date on the payer’s or agency’s terms and conditions. For updates on the PRF, check the HHS.gov site on reporting and auditing requirements.
Rely on Experienced Advisors
Audits can be intimidating and burdensome, even for organizations that have experienced them in the past. If you have received a notice of a third-party payer audit, or you just want to prepare for the possibility of an audit in the future, contact your CRI advisors. We will be happy to share our insights and experience.